Growing embryos - Embryo grading & PGT-A
In this article we will go over a few different topics:
- How many days should an embryo grow for?
- Embryo grading
- PGT-A
- Grading vs PGT-A - which one wins?
1. How many days should an embryo grow for?
When you conceive naturally, the fertilized egg takes a short but crucial several-day journey through the fallopian tube into the uterus. Throughout this journey, it develops more cells, and once it reaches the uterus, it makes its way to the uterus’s wall (the endometrium) where, if all goes well, it should attach.
During the IVF process, it’s up to the laboratory to grow the embryo before transferring it back into your uterus. To do this, the clinicians need to replicate the environment within the fallopian tube and uterus so that the embryo grows as it would inside the reproductive system. It’s not an easy job and until just a decade or so ago, laboratories could only grow (or ‘culture’) embryos to the ‘cleavage’ stage during which it has just five to eight cells.
Today, it’s possible to grow embryos to the ‘blastocyst’ stage, which is reached around day five to six. At this stage, the embryo has developed at least 60-100 cells and can be differentiated into a cell mass, which will become the fetus and an outer layer (or trophectoderm) which will become the placenta.
Only the most resilient embryos make it to the blastocyst stage and so it’s a good way to ensure your embryo has good developmental potential. However, it can mean losing a lot of embryos that cease to grow in the petri dish (known as ‘arresting’).
Having the option to grow your embryos to blastocyst stage does not necessarily mean you should. Despite knowing what we know about the journey the embryo takes before implanting, the debate is still ongoing over whether or not patients are more likely to succeed with blastocysts.
That most IVF cycles produce more cleavage embryos than blastocysts is where the difficulty lies. Of course, each embryo presents a possibility for a transfer and ultimately, one hopes, a pregnancy. The fewer the embryos, the fewer opportunities to transfer.
With that said, if you look at a single transfer then transferring a blastocyst does tend to increase chances. Below, we explain why this is.
Benefits of growing to blastocyst
Blastocyst stage is reached at approximately five days and can result in a higher success rate per transfer; multiple studies have found it to be about 1.5 times more likely to succeed. And we all know boosting odds as much as possible is preferable. Even if the transfer itself is not medically complicated, it can be emotionally draining and you want the greatest possible chance each time.
Sub-Genetic testing is possible
Embryos that have chromosomal abnormalities will most likely not lead to a live birth. It is possible to genetically test the embryos before the transfer, and this is best done at the blastocyst stage.
To screen the embryos, the clinic has to remove one or more cells from each embryo to test. It is more harmful to take cells from a cleavage stage embryo than a blastocyst embryo and so, if you choose to genetically test your embryos, they should be grown to blastocyst stage. If a clinic offers to test your cleavage stage embryos, this should set alarm bells ringing.
Whether genetic testing is the best course of action depends on a variety of factors. You can read more about that below.
When is the cleavage stage better?
More likely to be lost along the way when growing them to blastocyst stage. For those who produce fewer eggs and embryos, this can increase the risk of a canceled IVF cycle. In other words, you may end up with no transfer at all.
While many doctors have suggested that blastocysts are sturdier and therefore more likely to survive the freezing and thawing process, none of the data is convincing enough to guarantee this.
Essentially it comes down to whether you choose to have more attempts or optimize a particular one. Studies so far that have used a broad patient group and all their attempts (i.e. haven’t looked separately at groups with different issues), don’t draw strong enough conclusions about which route will increase your chances. Day five is typically preferred if the egg retrieval has resulted in many eggs and there are more embryos to work with, otherwise, cleavage is recommended. Before you make a decision, have an informed discussion with your doctor taking into account your history and diagnoses.
You may hear the argument that if an embryo doesn’t make it to blastocyst stage in the lab then it wouldn’t have resulted in a live birth if transferred to the uterus at cleavage stage. This is hypothetical because there’s simply no way of knowing what would have happened had the embryo been transferred earlier.
For those who don’t have the good luck to get pregnant quickly, you will soon realize that there is a degree of subjectivity with IVF. The decision about which stage to transfer the embryos can very much be based on your personal preferences, both physically and psychologically. Something that cannot be argued with is that a canceled cycle (when no embryo is transferred) will not lead to a live birth, and so it stands to follow that any transfer is better than no transfer at all. Or perhaps you have many failed transfers behind you and want to focus on optimizing chances for a specific transfer.
To summarize - it comes down to whether you would rather grow your embryos to blastocyst stage knowing you risk the entire IVF cycle being canceled (but will have insight into why it failed as you will know the embryo likely wasn’t “competent” enough); or rather maximize the number of attempts (including waiting the grueling two weeks to hear the result). If you opt for the latter, you’ve at least had a shot at pregnancy; however, if it fails you will be none the wiser about whether it was your uterus or embryo that was the problem (perhaps even both).
2. Embryo grading
Aside from deciding at which stage to transfer the embryos, the grading of the embryos is also a factor to consider - especially if you’re lucky enough to have many embryos to choose from.
Even if the grading can be expressed in different ways, clinics look at the same factors; two or three criteria are used by clinics to ‘grade’ an embryo to determine which one to transfer first. The criteria include looking at how fast the embryo is dividing and its morphological grading. This type of grading is somewhat subjective because it’s done by a human being, an embryologist, who could of course be more or less picky so to speak.
How well the embryo is dividing
Following successful fertilization, the sperm and egg grow into an embryo. From this point, the cells of the embryo should begin to rapidly divide; it’s the number of cells that determines the stage it has reached in its development (like cleavage or blastocyst). Most experts agree that the faster an embryo reaches a given stage, the higher the chance of success. For example, if an embryo reaches blastocyst stage in five days this is seen as a positive sign. However, embryos that reach blastocyst stage at six days shouldn’t be ruled out as they have been found to lead to live births. The same applies for patients considering a cleavage stage transfer: the quicker the embryo reaches cleavage stage, the more likely it’s considered to result in a live birth.
Morphological grading
Morphological grading refers to an assessment of how “expanded” the embryo is and how many cells comprise the inner mass and trophectoderm. This is often graded on a scale that includes one number followed by two letters:
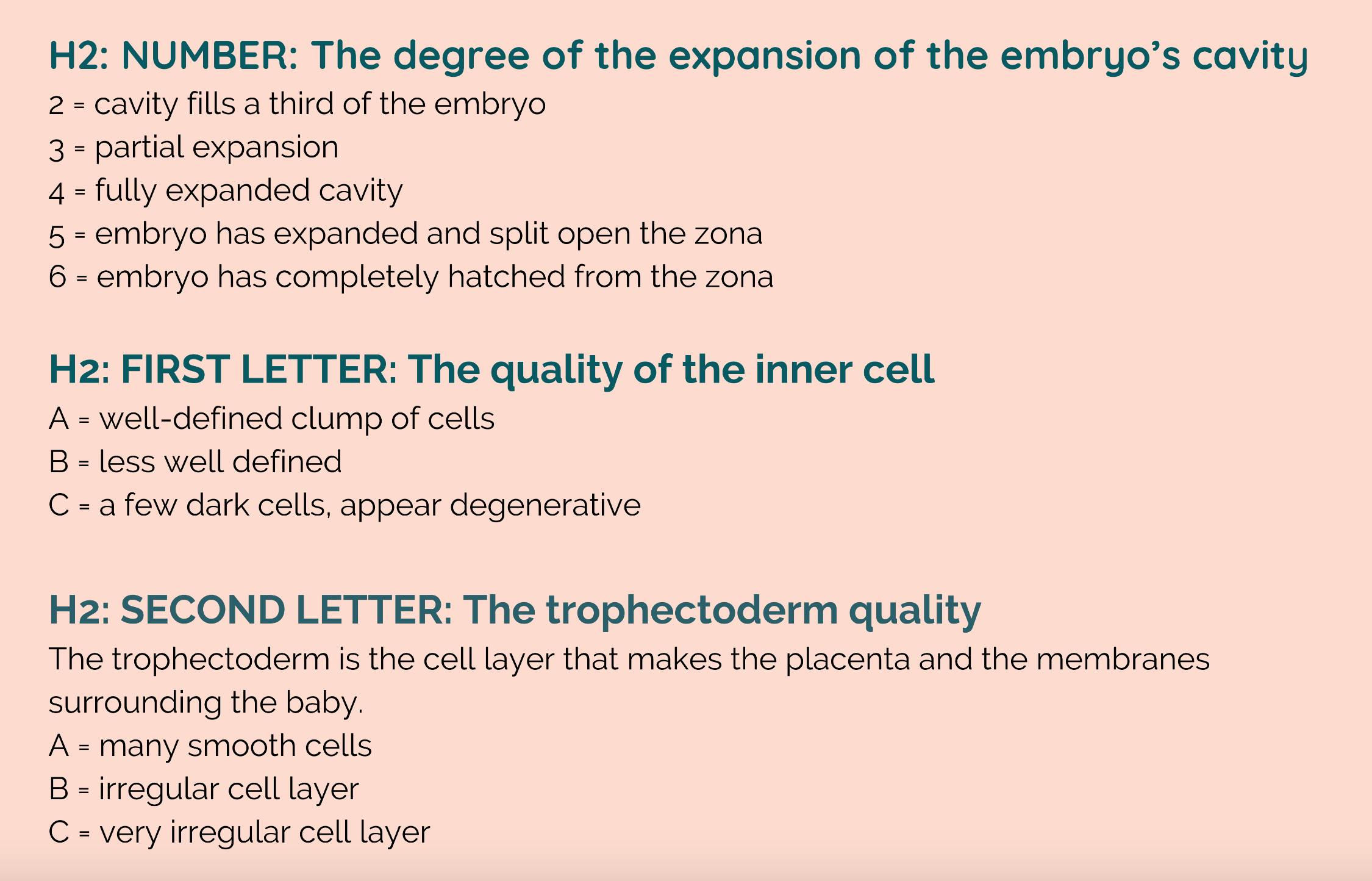
Expansion might be the first grade to be listed but that doesn’t make it the most important. The inner cell mass - the mass of cells that will eventually become the fetus - is the grade that best indicates the likelihood of success.
The nomenclature may differ between clinics but at the end of the day, they all refer to the same thing. If you feel unclear in any way, ask your clinic to explain it to you in simpler terms.
Morphological grades and outcomes
So, on the whole, how indicative are these three morphological scores of a successful pregnancy? It’s not an easy question to answer because there is a certain amount of interpretation when it comes to the grading. And other factors than embryo grading of course also play a role. That said, studies that have looked into this do tend to offer two conclusions:
- The better the embryo’s morphological traits, the more likely it will result in a viable pregnancy and live birth
- Despite this, it is possible for embryos with a high morphological grade to fail while less morphologically perfect embryos can succeed
Grading the inner cell mass and trophectoderm is subjective and different laboratories may have different guidelines for grading. For this reason, there is no way of generalizing how often an embryo will result in a live birth - only your clinic can explain what your grade means according to their system. It’s always possible to request an image of the embryos if you want to seek a second opinion from another laboratory.
It might be frustrating but there are no definitive answers. Morphological parameters are often subjective and as we have discussed, don’t necessarily predict with much accuracy whether or not your embryo will result in a live birth. If you have PGT-A results (which you can read more about below), these can give you an additional indication of success.
3. PGT-A
Preimplantation genetic testing for aneuploidy (often known as PGT-A, and previously known as PGS) is a genetic screening test performed on embryos to check for abnormalities in the number of chromosomes. Any chromosomally normal embryos are deemed fit to transfer.
Before we get started, it’s good to know that if your doctor hasn’t previously mentioned PGT-A, this is likely because it’s not allowed in your country of residence. For example, it’s not available in Sweden where doctors argue there is no proof that it improves pregnancy rates. This is true when you look at a broader group of patients; however, this may not be so if you break down the group into subgroups of patients with different ages and reproductive issues.
As is the case when deciding how long to grow an embryo, deciding whether a method is right for you is about weighing potential benefits against risks and costs.
How does PGT-A work?
When the embryo has reached the blastocyst stage, a few cells from the trophectoderm are carefully removed by embryologists and sent to a genetics laboratory for assessment. The lab will use a machine to predict the number of chromosomes for each embryo and report back to the fertility clinic. The report will show whether an embryo appears:
- ‘Euploid’: it has the right number of chromosomes and is more likely to lead to a live birth so should be transferred first
- ‘Aneuploid’: it has an incorrect number of chromosomes, in which case will not lead to the birth of a healthy baby
- ‘Mosaic’: the test was inconclusive and it couldn’t be determined whether the embryo was ‘euploid’ or ‘aneuploid’ but may still result in a live birth (although there may be risks)
Any results will be relayed back to the patient and this information can be used to decide which, if any, embryos should be transferred. If the decision is made to transfer an aneuploid or mosaic embryo, the risks and implications should be discussed with a genetic counselor.
Why use PGT-A?
Not all eggs and sperm have normal chromosomes and thus can’t lead to a viable pregnancy. It might be that sometimes they don’t fertilize or that the embryo ceases to grow, but some still become blastocysts. These are unlikely to implant and if they do, the pregnancy is likely to result in a miscarriage.
The number of eggs with normal chromosomes naturally declines as we age which is one of the reasons that it becomes harder to both conceive naturally and with IVF the older you are.
Pros of PGT-A
Better odds of a successful transfer and implantation: Embryos that have been PGT-A tested and approved are likelier to result in a successful transfer and subsequent implantation.
Less chance of miscarriage for older women: When it comes to older women in particular, who are more prone to having a higher share of chromosomally abnormal eggs, there is also less chance of a miscarriage if the eggs have been screened. This decrease is not as apparent among younger women.
Helps doctors diagnose other reproductive issues: If an embryo has been tested and approved at blastocyst stage and yet the transfer still fails (which most do), this may tell your doctor that the embryo was not the issue. They can then turn their attention to finding the true culprit, for example, an issue with the uterus. Keep in mind: If an embryo grows only to the cleavage stage before the transfer, it’s not guaranteed that it would have made it to the blastocyst stage. It could be that the embryo had a chromosomal abnormality, but it’s impossible to know with any certainty as it won’t have been tested. As a result, there’s no way to determine why the transfer may have failed.
Cons of PGT-A
It’s just a test: Ultimately, the PGT-A is a test and not a way to improve the quality of the embryos. While it can help to determine which embryos are best to transfer, genetic screening does not increase your chances of getting pregnant.
It may impact the viability of the embryo: While the data has been somewhat reassuring, there is still no definitive answer to whether PGT-A testing harms the embryo. The jury is still out, especially when you weigh up the risks of this technique against its benefits.
No test is 100% accurate: There have been concerns raised that the test may mistake a euploid embryo (a good-quality embryo) for an aneuploid (a low-quality embryo). If this occurs, it can be particularly problematic for older patients who already have difficulties producing good-quality eggs.
It’s expensive: While it would be wonderful if money was no object, most often it is. PGT-A can be costly which is something to be aware of when considering this option.
Conclusion
Taking all of the above into account, it can be concluded that PGT-A is normally recommended to women over the age of 35 or to those who have suffered repeated implantation failure or repeated miscarriages without any obvious cause or explanation.
4. Grading vs PGT-A - which one wins?
It’s not unheard of for an embryo to fail PGT-A testing but show other positive signs, such as growing quickly and reaching blastocyst stage at day five, and being graded highly on its morphology. And vice versa, an embryo might be assessed as good quality by the PGT-A test but receive a low morphological grade and be deemed unpromising by embryologists. In these instances, the consensus is that PGT-A testing is more indicative of success and that euploid embryos give the best possible chance.
2022-04-06

Evangelia Elenis, MD, PhD.
This text is fact checked by Evangelia Elenis, MD, PhD. Dr. Elenis is a chief physician in Obstetrics and Gynecology, and a subspecialist in Reproductive Medicine. She is a PhD and affiliated researcher at Uppsala University with postdoctoral studies at Harvard Medical School.
A mental health app for your fertility journey
Evidence-based self-care tools and facts. Supportive community. Treatment tracking.
Previous articles
Breaking the silence: Infertility and stress during stress awareness month
2025-04-14
Exciting news: Tilly is now part of Rhea
2025-03-31
How infertility impacts men's mental health and ways to cope
2024-11-22
Baby Loss Awareness Week: coming together to support those affected
2024-10-14
PCOS and mental health: a crucial connection
2024-09-25
How to support a friend struggling with involuntary childlessness: A guide for loved ones
2024-09-17