Fertilisation - ICSI or not?
When it comes to the fertilisation step in the IVF process, there’s more than one way to get the job done. To be really specific, there are two techniques that can be used to fertilise the eggs: conventional insemination or intra-cytoplasmic sperm injection (ICSI).
Conventional Insemination
This technique mirrors the way that natural fertilisation occurs by mixing mature eggs with sperm (the obvious difference being that it takes place in a petri dish!). The aim of the game, ultimately, is for one sperm to fertilise the egg.
Intracytoplasmic sperm injection (ICSI)
ICSI is a more delicate procedure in which an embryologist uses a tiny needle to inject a single sperm from a man’s semen sample into the center of the egg.
The ICSI procedure was designed to help couples experiencing issues associated with male factor infertility - when there are not enough healthy sperms. In these cases, fertilisation is the barrier to conceiving and ICSI can effectively help you to jump this hurdle.
But what about when there is only mild or even no male factor? And does the number of eggs that are retrieved affect the decision?
When you are in the midst of the IVF process, every available add-on may seem attractive, but although ICSI works wonders for some patients it’s not necessarily right for everyone. Therefore, it’s important to weigh out the pros and cons, taking into account your diagnoses and unique circumstances.
Whether to use ICSI or not is a decision that should be made together with your doctor, but being an informed patient can help you make better choices or at least feel more in control.
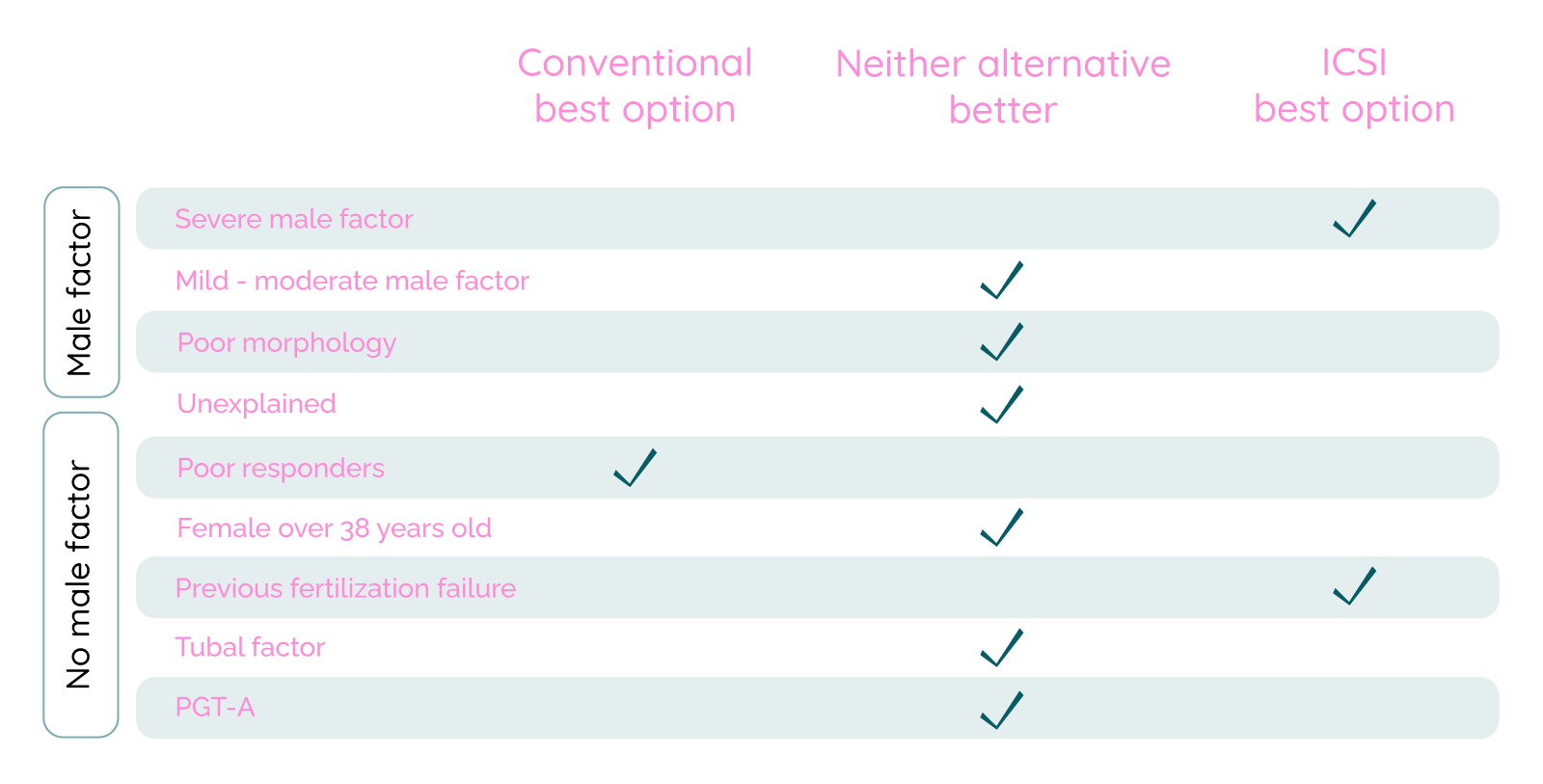
Benefits of ICSI per patient group
Let’s start with defining male factor infertility. It could be summarized as when the sperm of the intended father, for one reason or another, is unable to fertilise the egg. This can be indicated by a sperm sample where any or several of these factors deviate...
Concentration: Male factor infertility may occur if the volume of sperm produced per milliliter of semen is below 15 million.
Mobility: If fewer than 40% of sperm are able to move quickly or efficiently toward the egg.
Morphology: If less than 4-5% are the proper size and shape.
What’s morphology? It’s basically the shape of the sperm and whether it’s normal or not. We’ve all seen enough illustrations of sperm to at least imagine what a healthy sperm should look like when viewed under a microscope. The typical characteristics of a normally-formed sperm include a smooth oval-shaped head between 2.5-3.5 micrometers wide and 5-6 micrometers long, and a long, strong tail.
Group 1: Severe male factor
Azoospermia might look like a fun word but its meaning is far less pleasant. Put simply, it’s a fancy word that means ‘no sperm’, in which case, sperm have to be retrieved from nodules in the testicle using a surgical procedure.
In many cases of severe male factor, only a small amount of sperm can be retrieved and so conventional insemination is not an option. In instances when sperm is found and ICSI is used, 36% of the resulting IVF cycles lead to the birth of a healthy baby. It’s on these occasions that ICSI is most desirable.
Group 2: Moderate male factor
It may be the case that the male partner has low (but not no) sperm count. In such cases, you may wonder whether ICSI could be the solution. The answer is that there is (as of yet) no definitive answer. There aren’t sufficient studies to draw a satisfying conclusion, although ICSI does seem to reduce the risk of a frustrating event known as total fertilisation failure (TFF) in which no eggs are fertilised. However, it still isn’t clear if the rate of live births are any higher in this particular patient group.
Group 3: Poor morphology
When semen parameters, such as concentration and mobility, are otherwise good but a low percentage of the sperm (fewer than 5%) have a normal size and shape, the more reliable studies seem to show that ICSI does not improve the rate of live births.
Group 4: No male factor
There is nothing to suggest that ICSI increases success rates in cases where the male partner produces a healthy sperm sample. That’s not to say it’s case closed - the fact is, this group is too broad to draw any sufficient conclusions about whether ICSI is more effective than conventional insemination. The only way to accurately answer this question would be to study segments within the group as ICSI and conventional insemination vary by patient population.
Group 5: Female factors
No data conclusively proves that ICSI increases the chances for patients experiencing unexplained infertility, issues with fallopian tubes (known as tubal factor infertility or TFI), or women aged 38 or over (who are more likely to have low egg quality).
If a low number of eggs is retrieved, you may hear the term ‘poor responder’. In short, this means your ovaries have not responded well to stimulation. For so-called poor responders, ICSI may even reduce your chances. This is because when using ICSI in cases where fewer eggs are retrieved, there are not as many candidates for fertilisation as immature eggs (which account for ~20% of all eggs) can’t be used while 5-15% of eggs are destroyed during the ICSI process.
Group 6: Previous fertilisation failure
If you have previously experienced total fertilisation failure or low fertilisation (when less than 25% of eggs were fertilised), studies have suggested ICSI may be a good option regardless of other diagnosis.
Why has the use of ICSI increased in recent years?
As we have explained, in the majority of cases ICSI has not shown to improve your odds of conceiving. So why then, has the deployment of ICSI increased even when male factor infertility is not at play? The answer is that doctors and clinics fear that if your eggs don’t fertilize you will blame them for not using ICSI which has been shown to lower the risk of TFF.
The fact remains that ICSI does not make a pregnancy more likely. It can be very frustrating if no eggs fertilize and it’s natural to want to point the finger at the clinic. Clinics are well aware of this and so many use ICSI to safeguard despite knowing it doesn’t improve the chances of fertilization.
It should also be mentioned that there may be a financial incentive as ICSI comes with an added cost. With this in mind, make sure to have an informed conversation with your clinic before opting for one fertilization method over the other.
Does ICSI increase risk for birth defects?
Some studies suggest that, compared with conventional insemination, ICSI might lead to an increased incidence of chromosomal abnormalities, autism, intellectual disability, and birth defects. These outcomes may also be related to subfertility - in other words, a delay in conceiving - but there has also been speculation that it is a result of not allowing natural selection to do its job. These risks remain small and studies are often contradictory but it’s still only natural to feel concerned. However, if ICSI is the most promising option for fertilizing your eggs, then the benefits will likely outweigh the risks.
2022-02-15

Evangelia Elenis, MD, PhD.
This text is fact checked by Evangelia Elenis, MD, PhD. Dr. Elenis is a chief physician in Obstetrics and Gynecology, and a subspecialist in Reproductive Medicine. She is a PhD and affiliated researcher at Uppsala University with postdoctoral studies at Harvard Medical School.
A mental health app for your fertility journey
Evidence-based self-care tools and facts. Supportive community. Treatment tracking.
Previous articles
Breaking the silence: Infertility and stress during stress awareness month
2025-04-14
Exciting news: Tilly is now part of Rhea
2025-03-31
How infertility impacts men's mental health and ways to cope
2024-11-22
Baby Loss Awareness Week: coming together to support those affected
2024-10-14
PCOS and mental health: a crucial connection
2024-09-25
How to support a friend struggling with involuntary childlessness: A guide for loved ones
2024-09-17
